“The power of this multigenerational multiplier effect is tremendous, as a single surgeon in an LMIC setting can have a lifetime impact of over 400,000 cases through their training alone. As such, building surgical capacity through local training programs must be a part of any long-term global health initiative that seeks to close the unmet burden of surgical disease.”
– Cai, Lawrence MD; Meyers, Natalie MPH; Chang, James MD. Modeling the Lifetime Impact of Reconstructive Plastic Surgery Training: Implications for Building Capacity in Global Surgery.
At ReSurge, we focus on building reconstructive surgical capacity by training, funding, and scaling local surgical teams in low and middle-income countries. We believe this empowers surgeons to heal people with little to no access while training the next generation of surgeons to deliver and continue access to care. But why? And, does this have a substantial impact?
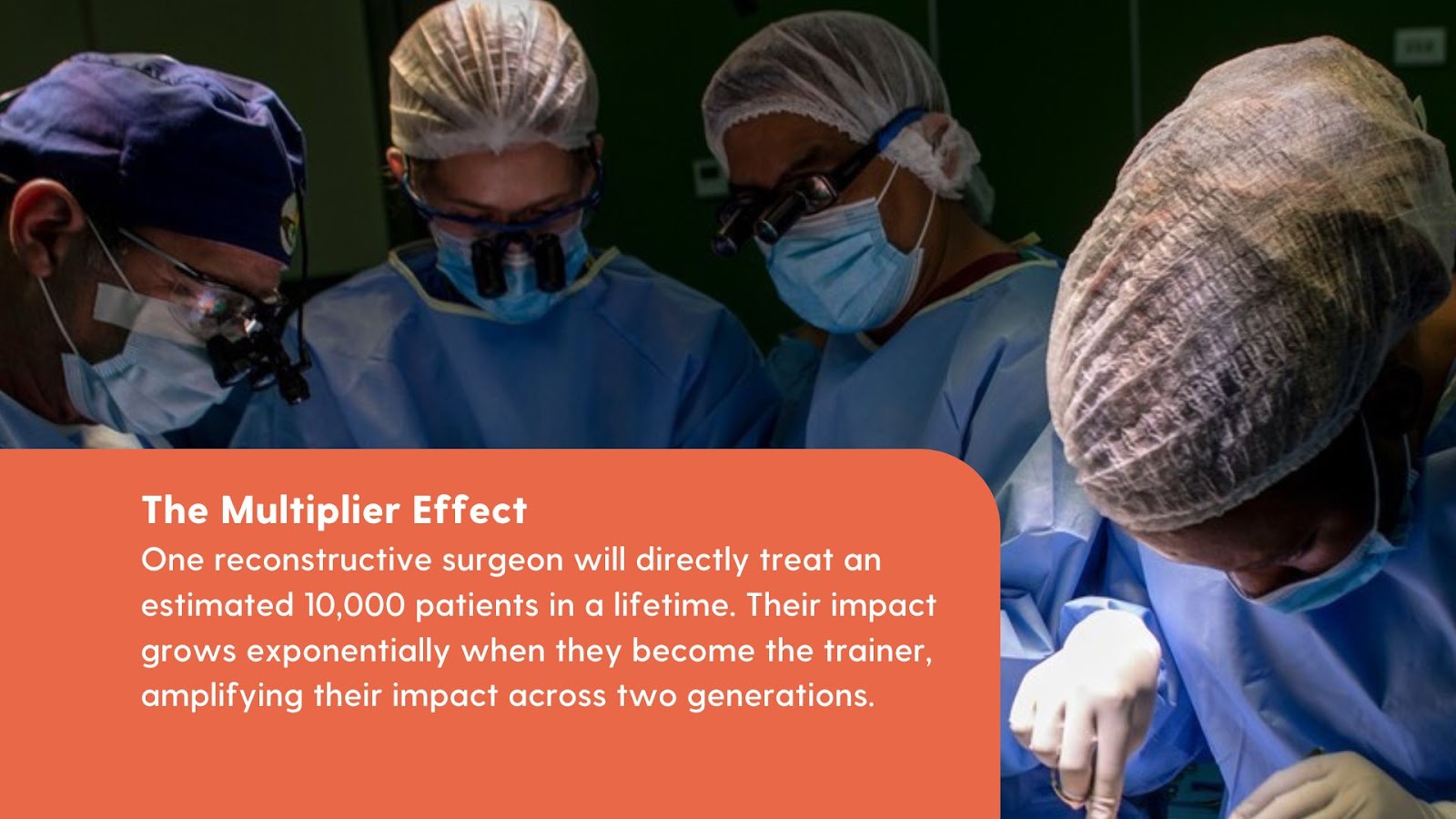
Published in the Plastic and Reconstructive Surgery – Global Open Journal, we’re excited to introduce a groundbreaking ReSurge and Stanford University study that unveils the first-ever framework for quantifying the impact of a single surgeon’s training across multiple generations of trainees. Co-authored by ReSurge Consulting Medical Officer & Chief of Plastic Surgery at Stanford, James Chang, MD, ReSurge Chief Program Officer Natalie Meyers, MPH, and Lawrence Cai, MD, Technical Program Manager at Google, our research finds that just one surgeon in a low-income country can treat 10,000 patients in their career and if they become a full-time surgeon-trainer, they can transform over 400,000 lives in their lifetime by their succeeding trainees — creating a substantial multiplier effect across generations!

What methods did we use?
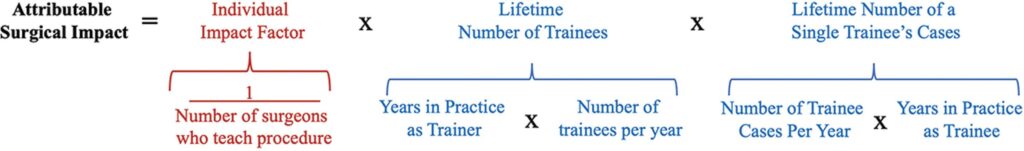
We developed this in three steps. We conducted a literature review to identify existing models for quantifying the impact of training across sectors that require hands-on training, including the US military, law, physical sciences, technology, humanities, arts, design, and public safety. We found that in all of these respective fields, there was a lack of models and/or methods for quantifying the impact of training across generations of trainees. This led us to create our model to estimate how much surgical training influences the number of surgeries done over two generations of trainees. We defined the impact of a surgeon’s training as the number of lifetime cases tied to that surgeon over two successive “generations” of trainees. Lastly, we quantitatively surveyed surgeons in high, low, and middle-income countries. Surgeons estimated the annual number of cases performed, the number of trainers who taught them the procedure, and the number of trainees expected to perform the procedure in the future.
What did we find?
First, we found no existing models for quantifying the multigenerational impact of training in surgery, medicine, or nonmedical fields, making our research the first of its kind.
Beyond the novelty of this research, we discovered a sizable impact in the first generation of training and an even greater impact in the second generation of training, highlighting the importance of a “multiplier effect” of training, particularly in LMIC settings.
To elaborate, the impact of training surgeons, particularly in under-resourced settings, is multi-tiered. These surgeons perform critical procedures that directly improve the lives of patients. They also train the next generation of local surgeons, who then train another generation of surgeons. We estimate a reconstructive surgeon will directly treat 10,000 patients throughout their career and if they become a surgeon-trainer, they can potentially transform over 400,000 lives. The power of this multigenerational multiplier effect is tremendous, as a single surgeon in an LMIC setting can have a lifetime impact of over 400,000 cases through their training. This is the multiplier effect quantified!
Beyond the Numbers: Why does this matter?
There is a profound shortage of surgeons in LMICs — thus creating an immense need to train surgeons locally. In 2014, Uganda had only three plastic surgeons in a population of 36 million people (one surgeon per 12 million people); Zambia (a population of 15 million people) had just one. In comparison, the United States has 12,000 plastic surgeons for a population of 330 million people (one surgeon per 0.027 million people).
Historically, global surgery efforts in LMICs have focused on the surgical mission model of bringing teams of surgeons, anesthesiologists, nurses, and other healthcare professionals to local hospitals and performing high volumes of cases in a relatively short time. While these teams have been able to deliver patient care, this has avoided addressing the inadequate surgical capacity at the local level. ReSurge International was a founder of the global surgery movement, and we were also one of the first organizations to move away from this fly-in model in the 1990s, investing in the training and capacity building of local surgical teams.

“This ground-breaking study confirms what we have been saying for decades — that training is the most effective and sustainable way to address the unmet surgical burden of disease in low-income countries.”
– Anna Santos, Chief Marketing Officer at ReSurge International
A train-the-trainer model represents a paradigmatic shift in global surgery — presenting a more sustainable and scalable way to deliver long-term access to surgical care in low and middle-income countries while empowering local surgeons and diversifying the global surgical workforce. We take pride in leading this transformative shift in global surgery and are even more honored to present tangible evidence of our method’s effectiveness.
This study is a glimpse into a broader vision at ReSurge and a broader discussion within global surgery. Our focus on training is multilayered. It empowers local surgeons to deliver quality care to patients who need it most. It results in a new generation of diverse and localized surgical teams and pioneers representative of the patients they serve, further contributing to improved patient outcomes. Overall, it creates a substantial ripple effect. A qualified surgeon has the power to train and develop more qualified surgeons — building local surgical capacity and future-proofing local surgical ecosystems.